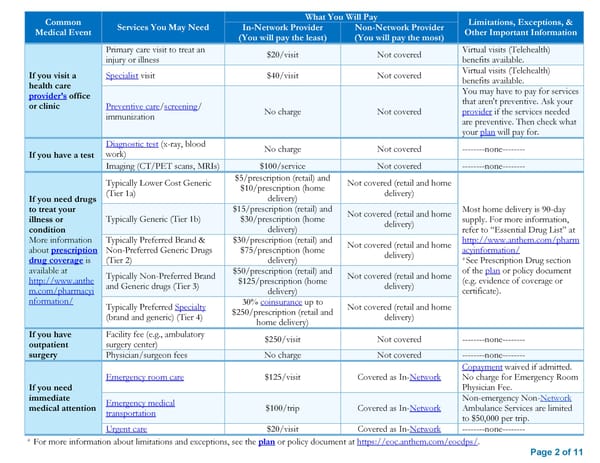
Common What You Will Pay Limitations, Exceptions, & Medical Event Services You May Need In-Network Provider Non-Network Provider Other Important Information (You will pay the least) (You will pay the most) Primary care visit to treat an $20/visit Not covered Virtual visits (Telehealth) injury or illness benefits available. If you visit a Specialist visit $40/visit Not covered Virtual visits (Telehealth) health care benefits available. provider’s office You may have to pay for services or clinic Preventive care/screening/ that aren't preventive. Ask your immunization No charge Not covered provider if the services needed are preventive. Then check what your plan will pay for. Diagnostic test (x-ray, blood No charge Not covered --------none-------- If you have a test work) Imaging (CT/PET scans, MRIs) $100/service Not covered --------none-------- Typically Lower Cost Generic $5/prescription (retail) and Not covered (retail and home (Tier 1a) $10/prescription (home delivery) If you need drugs delivery) to treat your $15/prescription (retail) and Not covered (retail and home Most home delivery is 90-day illness or Typically Generic (Tier 1b) $30/prescription (home delivery) supply. For more information, condition delivery) refer to “Essential Drug List” at More information Typically Preferred Brand & $30/prescription (retail) and Not covered (retail and home http://www.anthem.com/pharm about prescription Non-Preferred Generic Drugs $75/prescription (home delivery) acyinformation/ drug coverage is (Tier 2) delivery) *See Prescription Drug section available at Typically Non-Preferred Brand $50/prescription (retail) and Not covered (retail and home of the plan or policy document http://www.anthe and Generic drugs (Tier 3) $125/prescription (home delivery) (e.g. evidence of coverage or m.com/pharmacyi delivery) certificate). nformation/ Typically Preferred Specialty 30% coinsurance up to Not covered (retail and home (brand and generic) (Tier 4) $250/prescription (retail and delivery) home delivery) If you have Facility fee (e.g., ambulatory $250/visit Not covered --------none-------- outpatient surgery center) surgery Physician/surgeon fees No charge Not covered --------none-------- Copayment waived if admitted. Emergency room care $125/visit Covered as In-Network No charge for Emergency Room If you need Physician Fee. immediate Emergency medical Non-emergency Non-Network medical attention transportation $100/trip Covered as In-Network Ambulance Services are limited to $50,000 per trip. Urgent care $20/visit Covered as In-Network --------none-------- * For more information about limitations and exceptions, see the plan or policy document at https://eoc.anthem.com/eocdps/. Page 2 of 11
 Anthem Classic HMO 20/40/500 admit/250 OP SBC Page 1 Page 3
Anthem Classic HMO 20/40/500 admit/250 OP SBC Page 1 Page 3