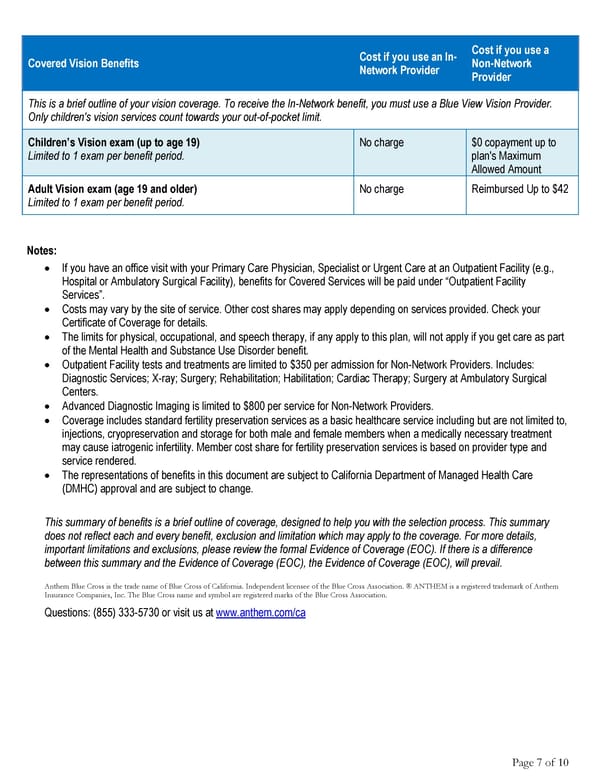
Cost if you use an In- Cost if you use a Covered Vision Benefits Network Provider Non-Network Provider This is a brief outline of your vision coverage. To receive the In-Network benefit, you must use a Blue View Vision Provider. Only children's vision services count towards your out-of-pocket limit. Children’s Vision exam (up to age 19) No charge $0 copayment up to Limited to 1 exam per benefit period. plan's Maximum Allowed Amount Adult Vision exam (age 19 and older) No charge Reimbursed Up to $42 Limited to 1 exam per benefit period. Notes: • If you have an office visit with your Primary Care Physician, Specialist or Urgent Care at an Outpatient Facility (e.g., Hospital or Ambulatory Surgical Facility), benefits for Covered Services will be paid under “Outpatient Facility Services”. • Costs may vary by the site of service. Other cost shares may apply depending on services provided. Check your Certificate of Coverage for details. • The limits for physical, occupational, and speech therapy, if any apply to this plan, will not apply if you get care as part of the Mental Health and Substance Use Disorder benefit. • Outpatient Facility tests and treatments are limited to $350 per admission for Non-Network Providers. Includes: Diagnostic Services; X-ray; Surgery; Rehabilitation; Habilitation; Cardiac Therapy; Surgery at Ambulatory Surgical Centers. • Advanced Diagnostic Imaging is limited to $800 per service for Non-Network Providers. • Coverage includes standard fertility preservation services as a basic healthcare service including but are not limited to, injections, cryopreservation and storage for both male and female members when a medically necessary treatment may cause iatrogenic infertility. Member cost share for fertility preservation services is based on provider type and service rendered. • The representations of benefits in this document are subject to California Department of Managed Health Care (DMHC) approval and are subject to change. This summary of benefits is a brief outline of coverage, designed to help you with the selection process. This summary does not reflect each and every benefit, exclusion and limitation which may apply to the coverage. For more details, important limitations and exclusions, please review the formal Evidence of Coverage (EOC). If there is a difference between this summary and the Evidence of Coverage (EOC), the Evidence of Coverage (EOC), will prevail. Anthem Blue Cross is the trade name of Blue Cross of California. Independent licensee of the Blue Cross Association. ® ANTHEM is a registered trademark of Anthem Insurance Companies, Inc. The Blue Cross name and symbol are registered marks of the Blue Cross Association. Questions: (855) 333-5730 or visit us at www.anthem.com/ca Page 7 of 10
 Anthem Classic PPO 500/30/50/20 Summary Page 6 Page 8
Anthem Classic PPO 500/30/50/20 Summary Page 6 Page 8