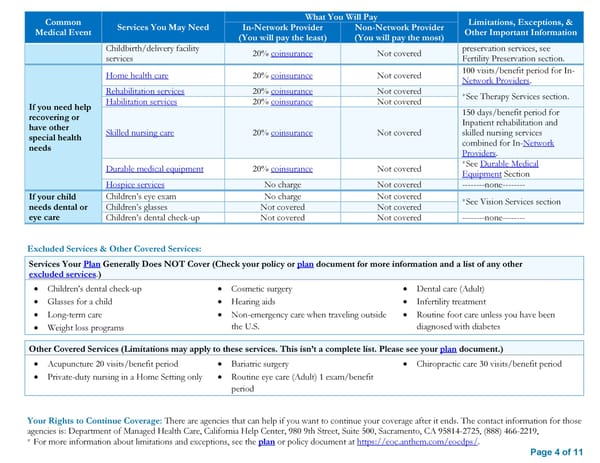
Common What You Will Pay Limitations, Exceptions, & Medical Event Services You May Need In-Network Provider Non-Network Provider Other Important Information (You will pay the least) (You will pay the most) Childbirth/delivery facility 20% coinsurance Not covered preservation services, see services Fertility Preservation section. Home health care 20% coinsurance Not covered 100 visits/benefit period for In- Network Providers. Rehabilitation services 20% coinsurance Not covered *See Therapy Services section. If you need help Habilitation services 20% coinsurance Not covered recovering or 150 days/benefit period for have other Inpatient rehabilitation and special health Skilled nursing care 20% coinsurance Not covered skilled nursing services needs combined for In-Network Providers. Durable medical equipment 20% coinsurance Not covered *See Durable Medical Equipment Section Hospice services No charge Not covered --------none-------- If your child Children’s eye exam No charge Not covered *See Vision Services section needs dental or Children’s glasses Not covered Not covered eye care Children’s dental check-up Not covered Not covered --------none-------- Excluded Services & Other Covered Services: Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Children’s dental check-up Cosmetic surgery Dental care (Adult) Glasses for a child Hearing aids Infertility treatment Long-term care Non-emergency care when traveling outside Routine foot care unless you have been Weight loss programs the U.S. diagnosed with diabetes Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture 20 visits/benefit period Bariatric surgery Chiropractic care 30 visits/benefit period Private-duty nursing in a Home Setting only Routine eye care (Adult) 1 exam/benefit period Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: Department of Managed Health Care, California Help Center, 980 9th Street, Suite 500, Sacramento, CA 95814-2725, (888) 466-2219, * For more information about limitations and exceptions, see the plan or policy document at https://eoc.anthem.com/eocdps/. Page 4 of 11
 Anthem EPO 3000/25/50/20 SBC Page 3 Page 5
Anthem EPO 3000/25/50/20 SBC Page 3 Page 5