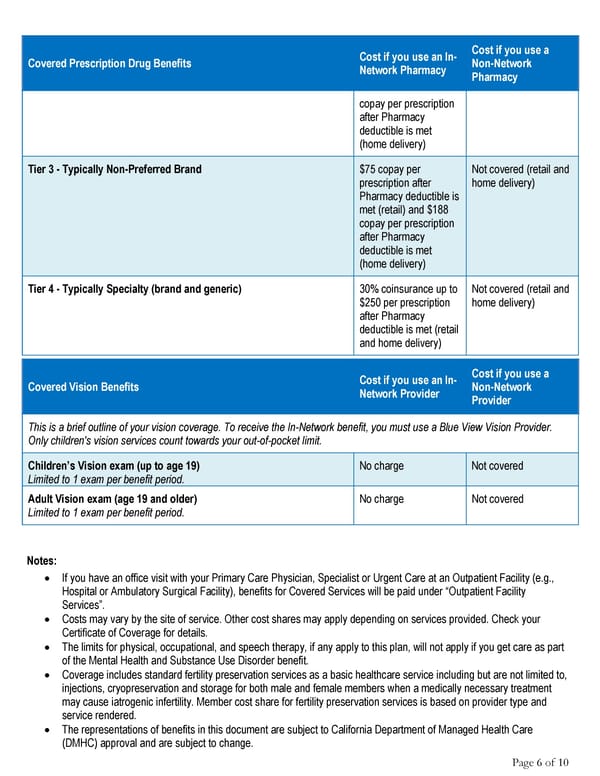
Cost if you use an In- Cost if you use a Covered Prescription Drug Benefits Network Pharmacy Non-Network Pharmacy copay per prescription after Pharmacy deductible is met (home delivery) Tier 3 - Typically Non-Preferred Brand $75 copay per Not covered (retail and prescription after home delivery) Pharmacy deductible is met (retail) and $188 copay per prescription after Pharmacy deductible is met (home delivery) Tier 4 - Typically Specialty (brand and generic) 30% coinsurance up to Not covered (retail and $250 per prescription home delivery) after Pharmacy deductible is met (retail and home delivery) Cost if you use an In- Cost if you use a Covered Vision Benefits Network Provider Non-Network Provider This is a brief outline of your vision coverage. To receive the In-Network benefit, you must use a Blue View Vision Provider. Only children's vision services count towards your out-of-pocket limit. Children’s Vision exam (up to age 19) No charge Not covered Limited to 1 exam per benefit period. Adult Vision exam (age 19 and older) No charge Not covered Limited to 1 exam per benefit period. Notes: • If you have an office visit with your Primary Care Physician, Specialist or Urgent Care at an Outpatient Facility (e.g., Hospital or Ambulatory Surgical Facility), benefits for Covered Services will be paid under “Outpatient Facility Services”. • Costs may vary by the site of service. Other cost shares may apply depending on services provided. Check your Certificate of Coverage for details. • The limits for physical, occupational, and speech therapy, if any apply to this plan, will not apply if you get care as part of the Mental Health and Substance Use Disorder benefit. • Coverage includes standard fertility preservation services as a basic healthcare service including but are not limited to, injections, cryopreservation and storage for both male and female members when a medically necessary treatment may cause iatrogenic infertility. Member cost share for fertility preservation services is based on provider type and service rendered. • The representations of benefits in this document are subject to California Department of Managed Health Care (DMHC) approval and are subject to change. Page 6 of 10
 Anthem Value Ded HMO 2000 30 60 25% Select HMO Summary Page 5 Page 7
Anthem Value Ded HMO 2000 30 60 25% Select HMO Summary Page 5 Page 7