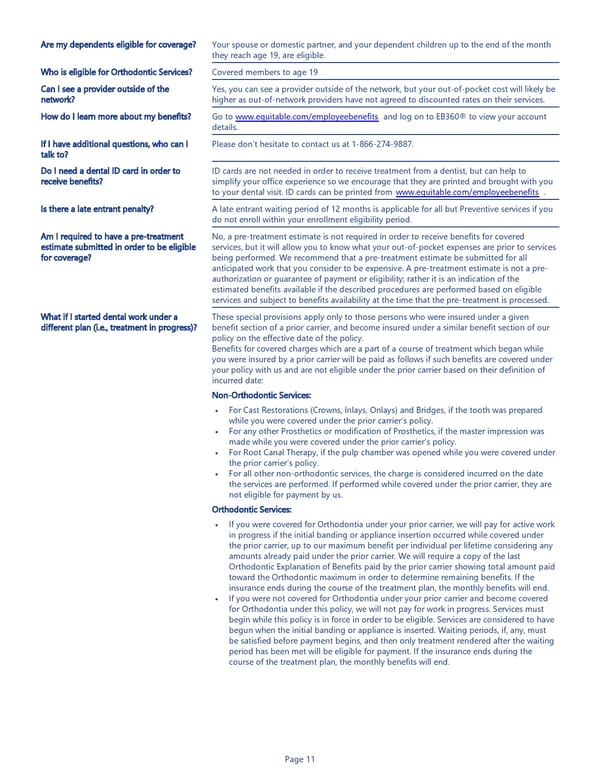
Page 11 Are my dependents eligible for coverage? Your spouse or domestic partner, and your dependent children up to the end of the month they reach age 19, are eligible. Who is eligible for Orthodontic Services? Covered members to age 19 Can I see a provider outside of the network? Yes, you can see a provider outside of the network, but your out-of-pocket cost will likely be higher as out-of-network providers have not agreed to discounted rates on their services. How do I learn more about my benefits? Go to www.equitable.com/employeebenefits and log on to EB360® to view your account details. If I have additional questions, who can I talk to? Please don’t hesitate to contact us at 1-866-274-9887. Do I need a dental ID card in order to receive benefits? ID cards are not needed in order to receive treatment from a dentist, but can help to simplify your office experience so we encourage that they are printed and brought with you to your dental visit. ID cards can be printed from www.equitable.com/employeebenefits . Is there a late entrant penalty? A late entrant waiting period of 12 months is applicable for all but Preventive services if you do not enroll within your enrollment eligibility period. Am I required to have a pre-treatment estimate submitted in order to be eligible for coverage? No, a pre-treatment estimate is not required in order to receive benefits for covered services, but it will allow you to know what your out-of-pocket expenses are prior to services being performed. We recommend that a pre-treatment estimate be submitted for all anticipated work that you consider to be expensive. A pre-treatment estimate is not a pre- authorization or guarantee of payment or eligibility; rather it is an indication of the estimated benefits available if the described procedures are performed based on eligible services and subject to benefits availability at the time that the pre-treatment is processed. What if I started dental work under a different plan (i.e., treatment in progress)? These special provisions apply only to those persons who were insured under a given benefit section of a prior carrier, and become insured under a similar benefit section of our policy on the effective date of the policy. Benefits for covered charges which are a part of a course of treatment which began while you were insured by a prior carrier will be paid as follows if such benefits are covered under your policy with us and are not eligible under the prior carrier based on their definition of incurred date: Non-Orthodontic Services: • For Cast Restorations (Crowns, Inlays, Onlays) and Bridges, if the tooth was prepared while you were covered under the prior carrier’s policy. • For any other Prosthetics or modification of Prosthetics, if the master impression was made while you were covered under the prior carrier’s policy. • For Root Canal Therapy, if the pulp chamber was opened while you were covered under the prior carrier’s policy. • For all other non-orthodontic services, the charge is considered incurred on the date the services are performed. If performed while covered under the prior carrier, they are not eligible for payment by us. Orthodontic Services: • If you were covered for Orthodontia under your prior carrier, we will pay for active work in progress if the initial banding or appliance insertion occurred while covered under the prior carrier, up to our maximum benefit per individual per lifetime considering any amounts already paid under the prior carrier. We will require a copy of the last Orthodontic Explanation of Benefits paid by the prior carrier showing total amount paid toward the Orthodontic maximum in order to determine remaining benefits. If the insurance ends during the course of the treatment plan, the monthly benefits will end. • If you were not covered for Orthodontia under your prior carrier and become covered for Orthodontia under this policy, we will not pay for work in progress. Services must begin while this policy is in force in order to be eligible. Services are considered to have begun when the initial banding or appliance is inserted. Waiting periods, if, any, must be satisfied before payment begins, and then only treatment rendered after the waiting period has been met will be eligible for payment. If the insurance ends during the course of the treatment plan, the monthly benefits will end. • • • • • •
 Dental Insurance Benefit Summary Page 10 Page 12
Dental Insurance Benefit Summary Page 10 Page 12