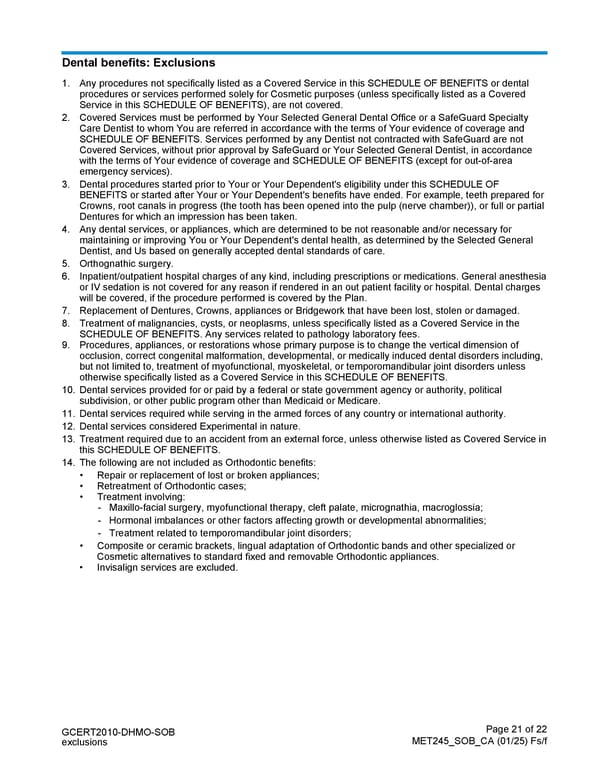
Page 21 of 22 MET245_SOB_CA (01/25) Fs/f GCERT2010-DHMO-SOB exclusions Dental benefits: Exclusions 1. Any procedures not specifically listed as a Covered Service in this SCHEDULE OF BENEFITS or dental procedures or services performed solely for Cosmetic purposes (unless specifically listed as a Covered Service in this SCHEDULE OF BENEFITS), are not covered. 2. Covered Services must be performed by Your Selected General Dental Office or a SafeGuard Specialty Care Dentist to whom You are referred in accordance with the terms of Your evidence of coverage and SCHEDULE OF BENEFITS. Services performed by any Dentist not contracted with SafeGuard are not Covered Services, without prior approval by SafeGuard or Your Selected General Dentist, in accordance with the terms of Your evidence of coverage and SCHEDULE OF BENEFITS (except for out-of-area emergency services). 3. Dental procedures started prior to Your or Your Dependent's eligibility under this SCHEDULE OF BENEFITS or started after Your or Your Dependent's benefits have ended. For example, teeth prepared for Crowns, root canals in progress (the tooth has been opened into the pulp (nerve chamber)), or full or partial Dentures for which an impression has been taken. 4. Any dental services, or appliances, which are determined to be not reasonable and/or necessary for maintaining or improving You or Your Dependent's dental health, as determined by the Selected General Dentist, and Us based on generally accepted dental standards of care. 5. Orthognathic surgery. 6. Inpatient/outpatient hospital charges of any kind, including prescriptions or medications. General anesthesia or IV sedation is not covered for any reason if rendered in an out patient facility or hospital. Dental charges will be covered, if the procedure performed is covered by the Plan. 7. Replacement of Dentures, Crowns, appliances or Bridgework that have been lost, stolen or damaged. 8. Treatment of malignancies, cysts, or neoplasms, unless specifically listed as a Covered Service in the SCHEDULE OF BENEFITS. Any services related to pathology laboratory fees. 9. Procedures, appliances, or restorations whose primary purpose is to change the vertical dimension of occlusion, correct congenital malformation, developmental, or medically induced dental disorders including, but not limited to, treatment of myofunctional, myoskeletal, or temporomandibular joint disorders unless otherwise specifically listed as a Covered Service in this SCHEDULE OF BENEFITS. 10. Dental services provided for or paid by a federal or state government agency or authority, political subdivision, or other public program other than Medicaid or Medicare. 11. Dental services required while serving in the armed forces of any country or international authority. 12. Dental services considered Experimental in nature. 13. Treatment required due to an accident from an external force, unless otherwise listed as Covered Service in this SCHEDULE OF BENEFITS. 14. The following are not included as Orthodontic benefits: • Repair or replacement of lost or broken appliances; • Retreatment of Orthodontic cases; • Treatment involving: - Maxillo-facial surgery, myofunctional therapy, cleft palate, micrognathia, macroglossia; - Hormonal imbalances or other factors affecting growth or developmental abnormalities; - Treatment related to temporomandibular joint disorders; • Composite or ceramic brackets, lingual adaptation of Orthodontic bands and other specialized or Cosmetic alternatives to standard fixed and removable Orthodontic appliances. • Invisalign services are excluded.
 Schedule of Benefits Page 20 Page 22
Schedule of Benefits Page 20 Page 22