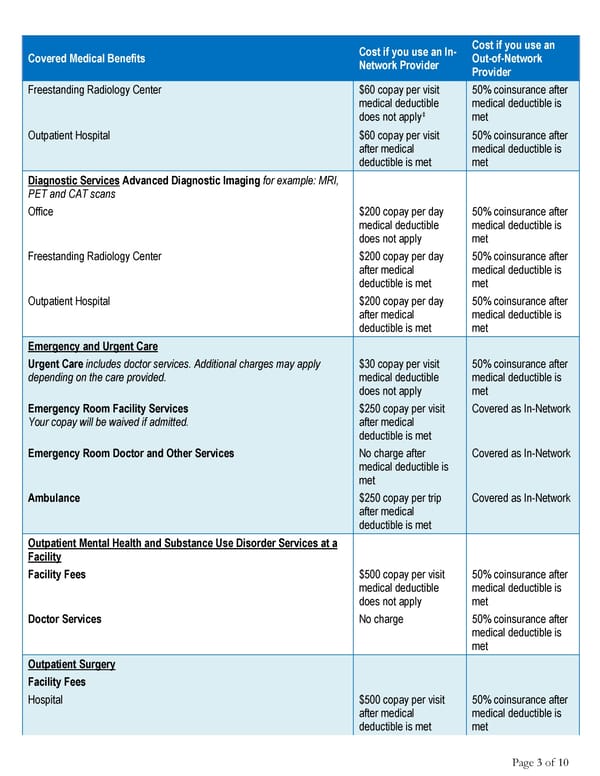
Page 3 of 10 Covered Medical Benefits Cost if you use an In- Network Provider Cost if you use an Out-of-Network Provider Freestanding Radiology Center $60 copay per visit medical deductible does not apply‡ 50% coinsurance after medical deductible is met Outpatient Hospital $60 copay per visit after medical deductible is met 50% coinsurance after medical deductible is met Diagnostic Services Advanced Diagnostic Imaging for example: MRI, PET and CAT scans Office $200 copay per day medical deductible does not apply 50% coinsurance after medical deductible is met Freestanding Radiology Center $200 copay per day after medical deductible is met 50% coinsurance after medical deductible is met Outpatient Hospital $200 copay per day after medical deductible is met 50% coinsurance after medical deductible is met Emergency and Urgent Care Urgent Care includes doctor services. Additional charges may apply depending on the care provided. $30 copay per visit medical deductible does not apply 50% coinsurance after medical deductible is met Emergency Room Facility Services Your copay will be waived if admitted. $250 copay per visit after medical deductible is met Covered as In-Network Emergency Room Doctor and Other Services No charge after medical deductible is met Covered as In-Network Ambulance $250 copay per trip after medical deductible is met Covered as In-Network Outpatient Mental Health and Substance Use Disorder Services at a Facility Facility Fees $500 copay per visit medical deductible does not apply 50% coinsurance after medical deductible is met Doctor Services No charge 50% coinsurance after medical deductible is met Outpatient Surgery Facility Fees Hospital $500 copay per visit after medical deductible is met 50% coinsurance after medical deductible is met
 Anthem Blue Cross: Summary of Benefits Page 2 Page 4
Anthem Blue Cross: Summary of Benefits Page 2 Page 4