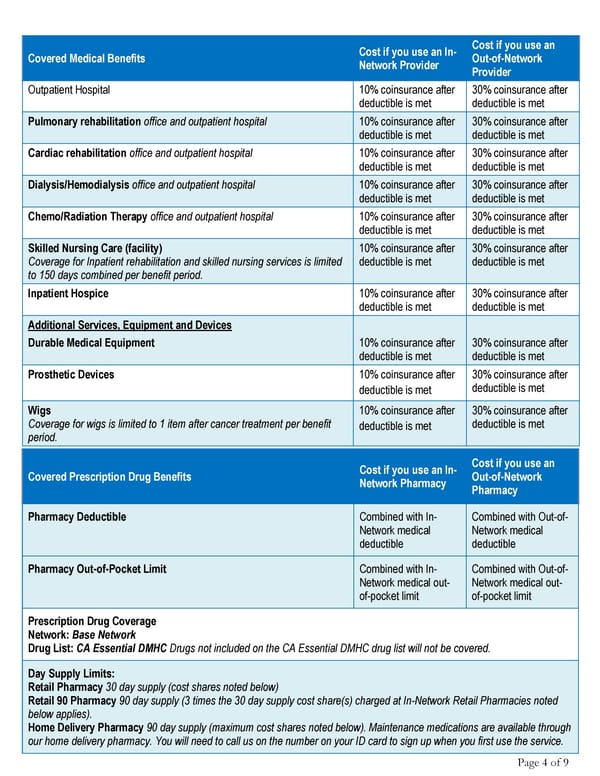
Page 4 of 9 Covered Medical Benefits Cost if you use an In- Network Provider Cost if you use an Out-of-Network Provider Outpatient Hospital 10% coinsurance after deductible is met 30% coinsurance after deductible is met Pulmonary rehabilitation office and outpatient hospital 10% coinsurance after deductible is met 30% coinsurance after deductible is met Cardiac rehabilitation office and outpatient hospital 10% coinsurance after deductible is met 30% coinsurance after deductible is met Dialysis/Hemodialysis office and outpatient hospital 10% coinsurance after deductible is met 30% coinsurance after deductible is met Chemo/Radiation Therapy office and outpatient hospital 10% coinsurance after deductible is met 30% coinsurance after deductible is met Skilled Nursing Care (facility) Coverage for Inpatient rehabilitation and skilled nursing services is limited to 150 days combined per benefit period. 10% coinsurance after deductible is met 30% coinsurance after deductible is met Inpatient Hospice 10% coinsurance after deductible is met 30% coinsurance after deductible is met Additional Services, Equipment and Devices Durable Medical Equipment 10% coinsurance after deductible is met 30% coinsurance after deductible is met Prosthetic Devices 10% coinsurance after deductible is met 30% coinsurance after deductible is met Wigs Coverage for wigs is limited to 1 item after cancer treatment per benefit period. 10% coinsurance after deductible is met 30% coinsurance after deductible is met Covered Prescription Drug Benefits Cost if you use an In- Network Pharmacy Cost if you use an Out-of-Network Pharmacy Pharmacy Deductible Combined with In- Network medical deductible Combined with Out-of- Network medical deductible Pharmacy Out-of-Pocket Limit Combined with In- Network medical out- of-pocket limit Combined with Out-of- Network medical out- of-pocket limit Prescription Drug Coverage Network: Base Network Drug List: CA Essential DMHC Drugs not included on the CA Essential DMHC drug list will not be covered. Day Supply Limits: Retail Pharmacy 30 day supply (cost shares noted below) Retail 90 Pharmacy 90 day supply (3 times the 30 day supply cost share(s) charged at In-Network Retail Pharmacies noted below applies). Home Delivery Pharmacy 90 day supply (maximum cost shares noted below). Maintenance medications are available through our home delivery pharmacy. You will need to call us on the number on your ID card to sign up when you first use the service.
 Summary of Benefits Page 3 Page 5
Summary of Benefits Page 3 Page 5