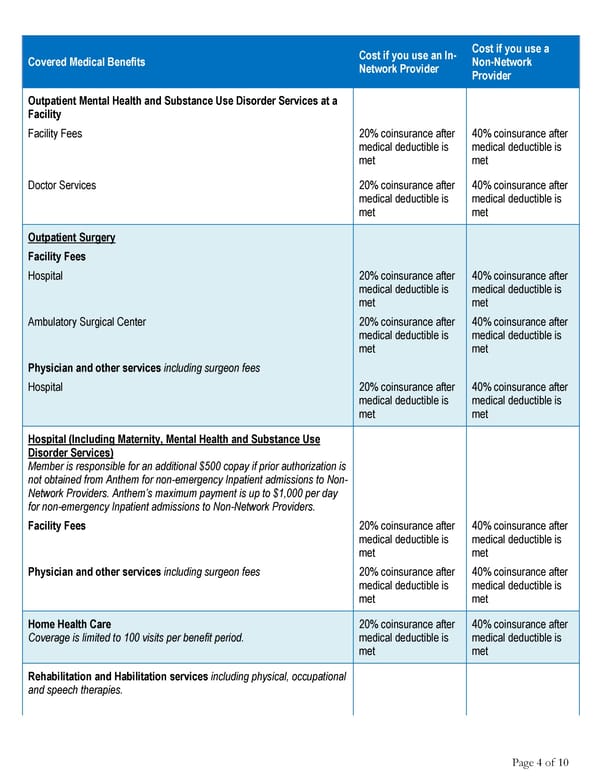
Cost if you use an In- Cost if you use a Covered Medical Benefits Network Provider Non-Network Provider Outpatient Mental Health and Substance Use Disorder Services at a Facility Facility Fees 20% coinsurance after 40% coinsurance after medical deductible is medical deductible is met met Doctor Services 20% coinsurance after 40% coinsurance after medical deductible is medical deductible is met met Outpatient Surgery Facility Fees Hospital 20% coinsurance after 40% coinsurance after medical deductible is medical deductible is met met Ambulatory Surgical Center 20% coinsurance after 40% coinsurance after medical deductible is medical deductible is met met Physician and other services including surgeon fees Hospital 20% coinsurance after 40% coinsurance after medical deductible is medical deductible is met met Hospital (Including Maternity, Mental Health and Substance Use Disorder Services) Member is responsible for an additional $500 copay if prior authorization is not obtained from Anthem for non-emergency Inpatient admissions to Non- Network Providers. Anthem’s maximum payment is up to $1,000 per day for non-emergency Inpatient admissions to Non-Network Providers. Facility Fees 20% coinsurance after 40% coinsurance after medical deductible is medical deductible is met met Physician and other services including surgeon fees 20% coinsurance after 40% coinsurance after medical deductible is medical deductible is met met Home Health Care 20% coinsurance after 40% coinsurance after Coverage is limited to 100 visits per benefit period. medical deductible is medical deductible is met met Rehabilitation and Habilitation services including physical, occupational and speech therapies. Page 4 of 10
 Anthem Classic PPO 500/30/50/20 Summary Page 3 Page 5
Anthem Classic PPO 500/30/50/20 Summary Page 3 Page 5