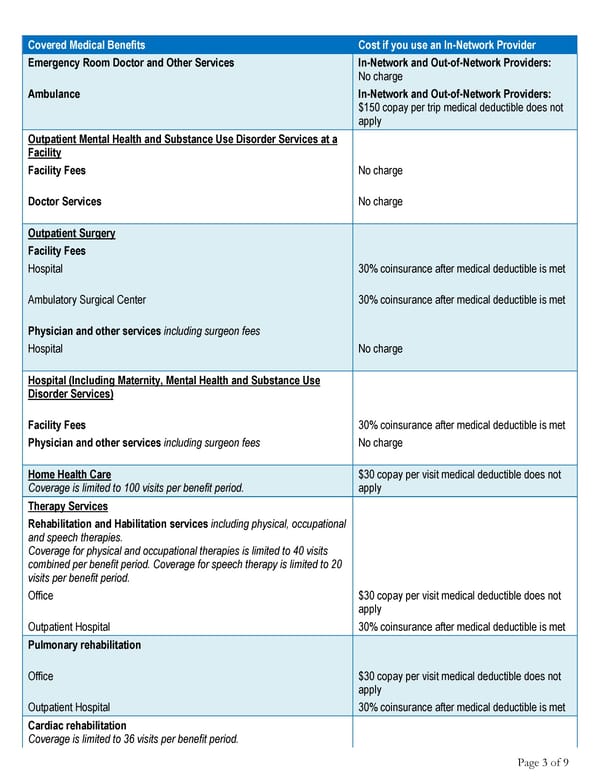
Page 3 of 9 Covered Medical Benefits Cost if you use an In-Network Provider Emergency Room Doctor and Other Services In-Network and Out-of-Network Providers: No charge Ambulance In-Network and Out-of-Network Providers: $150 copay per trip medical deductible does not apply Outpatient Mental Health and Substance Use Disorder Services at a Facility Facility Fees No charge Doctor Services No charge Outpatient Surgery Facility Fees Hospital 30% coinsurance after medical deductible is met Ambulatory Surgical Center 30% coinsurance after medical deductible is met Physician and other services including surgeon fees Hospital No charge Hospital (Including Maternity, Mental Health and Substance Use Disorder Services) Facility Fees 30% coinsurance after medical deductible is met Physician and other services including surgeon fees No charge Home Health Care Coverage is limited to 100 visits per benefit period. $30 copay per visit medical deductible does not apply Therapy Services Rehabilitation and Habilitation services including physical, occupational and speech therapies. Coverage for physical and occupational therapies is limited to 40 visits combined per benefit period. Coverage for speech therapy is limited to 20 visits per benefit period. Office $30 copay per visit medical deductible does not apply Outpatient Hospital 30% coinsurance after medical deductible is met Pulmonary rehabilitation Office $30 copay per visit medical deductible does not apply Outpatient Hospital 30% coinsurance after medical deductible is met Cardiac rehabilitation Coverage is limited to 36 visits per benefit period.
 Your Summary of Benefits - Anthem Blue Cross Page 2 Page 4
Your Summary of Benefits - Anthem Blue Cross Page 2 Page 4